TMJ Disorders & Bruxism
What is the temporomandibular joint (TMJ)?
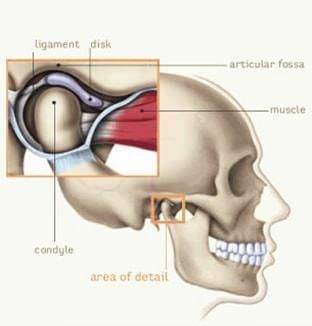
The temporomandibular joint (TMJ) is the small joint in front of the ear where the skull is met by the lower jaw (mandible).
The TMJ is the most constantly used joint in the body and the only joint that hinges and slides as part of its normal function.
It makes sense that a joint with such complex movements and is the most used will likely suffer from disorders during its lifetime if the balance and synchronisation of these moving parts are affected.
The left and right TMJs must work together to coordinate swallowing, opening and closing the jaws, aligning the teeth, chewing food and speaking.
What are temporomandibular disorders (TMD)?
Temporomandibular Disorders (TMD) is a collective term for various clinical symptoms and signs involving the muscles of mastication (chewing) and the internal structures of the temporomandibular joint itself.
The TMJ is close to the brain above, the external and internal ear structures behind, and the muscles involved with chewing on either side, so the presenting symptoms of TMJ disorders can involve any or all of these structures.
How Do TMJ Disorders Impact Your Anatomy and Health?
TMJ Disorders can cause various symptoms that can significantly impact your quality of life, making it difficult to enjoy everyday activities such as eating and speaking. In some cases, TMJ Disorders can also lead to long-term damage to the jaw joint and surrounding structures, making early diagnosis and treatment essential.
Types of Common TMJ Disorders
60-70% of the general population will have one symptom or sign of TMD, but that does not mean they all have a disorder. Of all the TMD presentations to the Dentist or Specialist, they will fall into four main categories:
- 80% are muscle-related issues
- 15% are joint or internal derangement of joint structures
- 4% are osteoarthritis
- 1% are other degenerative joint diseases or significant pathology
Risk Factors and Causes of TMJ Disorders
The exact causes of TMD are not fully understood, but several factors can contribute to the development of these disorders. These factors include:
- Jaw injuries: Trauma to the jaw joint, such as a blow to the face or whiplash, can cause TMD.
- Dental problems: Dental issues such as misaligned teeth, missing teeth, or a bad bite can pressure the jaw joint and lead to TMD.
- Arthritis: Osteoarthritis and rheumatoid arthritis can cause inflammation and damage to the jaw joint.
- Stress: Emotional or physical stress can cause muscle tension and lead to TMD.
- Habits: Teeth grinding, jaw clenching, and nail-biting can pressure the jaw joint and lead to TMD.
Symptoms of TMJ Disorders
The symptoms of TMD can vary depending on the type and severity of the condition. Some common symptoms include
- Pain or tenderness in the jaw joint, face, neck, and shoulders.
- Clicking, popping, or grating sounds in the jaw joint when opening or closing the mouth.
- Difficulty opening or closing the mouth or locking the jaw joint.
- Headaches, earaches, dizziness, and ringing in the ears.
- Teeth grinding or clenching (bruxism).
- Facial swelling or facial asymmetry.
- Fatigue or tiredness in the jaw muscles.
Having one or more of these symptoms is quite common. However, getting your dentist's review is still important to get the appropriate investigations and imaging to achieve the correct diagnosis.
Stages of TMJ Disorders
TMD can progress through different stages, and the severity of symptoms can increase over time. The stages of TMD are as follows:
- Stage 1: Early stage – Minimal discomfort, occasional clicking or popping of the jaw joint, no limitations in jaw movements.
- Stage 2: Mild dysfunction – More frequent clicking or popping sounds, occasional pain or discomfort, mild limitations in jaw movements.
- Stage 3: Moderate dysfunction – Frequent clicking or popping sounds, moderate pain or discomfort, noticeable limitations in jaw movements.
- Stage 4: Severe dysfunction – Chronic pain, significant limitations in jaw movements, difficulty eating and talking.
It's essential to seek treatment from a qualified dentist if you experience any symptoms of TMD. Early diagnosis and treatment can help prevent the progression of TMD and improve your oral health and quality of life.
Diagnosis of TMJ Disorders
Your dentist will ask you about your symptoms and medical history and perform a physical examination.
The physical exam involves:
- Examining your teeth, jaw joints, facial muscles and head.
- Palpation of the jaw joint, facial muscles and head.
- Listening to clicking/popping sounds when you open your jaw.
Other tests your dentist may order:
- X-rays: Panoramic dental X-rays can show a wide view of jaws, teeth and roots.
- Tomogram: This type of x-ray shows different sections throughout the joint. It is used to diagnose arthritis and injuries.
- CT scan: This type of scan uses a computer to make internal pictures of the joint and helps to see bony details.
- MRI scan: Magnetic and radio waves picture the jaw joint.
What are the Treatments for TMJ Disorders?
Home Remedy
You can apply warm compresses over the painful area. Exercise your lower jaw by moving it side to side and trying to open and close your mouth. Try this after you apply a warm compress for 20 minutes.
Medications:
Muscle relaxant medicines are prescribed to help control muscle spasms and pain. Non-Steroidal Anti-inflammatory Drugs (NSAIDs) like aspirin or ibuprofen will reduce pain and swelling.
Low-dose antidepressants may also be given for pain modification.
Physical Therapy,
Physical Therapy exercises help relax your muscles and improve jaw movements. Physiotherapists use the Transcutaneous Electrical Nerve Stimulation (TENS) unit and ultrasound, which promotes tissue healing and helps relax your muscles.
Lifestyle Changes
Include avoiding hard or chewy foods, practising stress reduction techniques, and avoiding jaw overuse.
Splint Therapy
This treatment is suggested to eliminate the effects of clenching or grinding the teeth. A splint is an appliance that fits over the chewing surfaces of your upper and lower teeth. It is worn for almost 1-3 months or more.
Orthodontic Correction
If your TMJ disorder is caused by how your teeth fit together, it helps if the occlusion is corrected. Orthodontic braces will be used to reposition your teeth. If there is malalignment in the jaws, orthognathic surgery is required to change the positions of the jaw bones.
Surgery
Surgery is the last resort when all other treatment methods have failed. Surgery may be necessary if muscle spasms increase in frequency, TMJ has become arthritic or when there is an injury to the joint.
Types of TMJ Surgery
- Arthrocentesis: This is performed under general anaesthesia or IV sedation. In this procedure, the surgeon injects local anaesthesia and fluids inside the joint to flush out inflamed fluids. It is indicated in cases where the articular disc has adhered to the temporal fossa. This procedure requires approximately 15 minutes.
- TMJ replacement: This is indicated in cases of badly damaged joints from severe degenerative disease, advanced rheumatoid arthritis and congenital deformity of TMJ.
TMJ Disorders Prevention
Preventing TMJ disorders can include the following measures:
- Stop grinding or clenching habits or use night guards (splints).
- Limit excessive jaw movements.
- Learn effective ways to overcome stress.
- Avoid eating hard foods.
Bruxism
What is Bruxism?
Bruxism is a condition characterised by the clenching and grinding of teeth, typically during sleep. It can also occur during waking hours, although this is less common. Bruxism can affect people of all ages but is most common in children and young adults.
What are the Symptoms of Bruxism?
Some of the symptoms of bruxism include:
- Grinding or clenching of teeth during sleep
- Headaches, earaches, or facial pain
- Soreness or stiffness in the jaw or neck muscles
- Difficulty opening or closing the mouth
- Chipped, cracked, or worn-down teeth
- Tooth sensitivity
What are the Causes of Bruxism?
The exact cause of bruxism is not always clear, but it is thought to be linked to a combination of factors, including stress, anxiety, an abnormal bite, and sleep disorders such as sleep apnea. In some cases, bruxism may also be a side effect of certain medications or substances, such as caffeine or alcohol.
While not always serious, bruxism can cause dental problems and discomfort over time. So, speaking with your dentist if you suspect you may have bruxism is important.
When Should Bruxism Be Treated?
Here are some of the main reasons why bruxism should be promptly treated:
- Pain or discomfort: If bruxism is causing pain or discomfort in the teeth, jaw, or neck, it may be worth seeking treatment. Over time, bruxism can cause damage to teeth, resulting in tooth sensitivity, pain, and difficulty chewing.
- Tooth damage: If bruxism is causing visible damage to teeth, such as chips or fractures, treatment may be necessary to prevent further damage.
- Sleep disturbance: Bruxism can disturb sleep, both for the person with bruxism and their partner. If this is the case, treatment may be necessary to improve sleep quality.
- Severity: The severity of bruxism can vary from person to person. Treatment may be necessary if it is severe enough to cause significant damage or pain.
- Underlying medical conditions: Bruxism can be caused by underlying medical conditions, such as sleep apnea, anxiety, or stress. In these cases, treating the underlying condition may also help alleviate bruxism.
What is the Treatment for Bruxism?
Several treatments for bruxism include
- Mouthguards or splints: A mouthguard or splint can be worn at night to help protect the teeth from grinding and clenching. These devices can be custom-made by a dentist or purchased over the counter.
- Stress management techniques: Bruxism can be caused or worsened by stress and anxiety, so practising stress management techniques such as meditation, yoga, or counselling may help reduce bruxism.
- Muscle relaxation exercises: Exercises focusing on relaxing the jaw and facial muscles can help reduce bruxism. These exercises may include gentle jaw stretches, massages, or warm compresses.
- Dental corrections: In some cases, dental corrections such as reshaping or realigning teeth may be recommended to help alleviate bruxism.
- Medications: In certain cases, medications such as muscle relaxants, antidepressants, or Botox injections may be prescribed to help reduce bruxism.
Relationship between TMJ Disorder and Bruxism?
TMJ Disorder and bruxism are two conditions that can be closely related. Bruxism can contribute to the development or exacerbation of TMJ Disorder.
When a person with bruxism clenches or grinds their teeth, it puts pressure on the TMJ and surrounding muscles, leading to inflammation and pain. Over time, this can contribute to the development of TMJ Disorder.
On the other hand, TMJ Disorder can also contribute to bruxism. When the TMJ is misaligned or not functioning properly, it can cause a person to grind or clench their teeth to compensate for the discomfort or pain.
Therefore, it is important to treat both bruxism and TMJ Disorder to manage and prevent the progression of these conditions. Consult a dental or medical professional who can evaluate your case and recommend the most appropriate treatment option.
About Us
We are a full service family dental practice.
Family Dental Practice has proudly been recognised as one of Australia’s top dentists
Practice Hours
- Mon, Tue, Wed, Fri
- -
- Thursday
- Closed
- Saturday
- -
- Sunday
- Closed
All Rights Reserved | Family Dental Practice